What is IBS (Irritable Bowel Syndrome)?
Irritable Bowel Syndrome (IBS) is a functional disorder of the lower bowel that affects more women than men, usually between the ages of 20 – 40 years. It is called a syndrome because IBS can present a wide range of correlated symptoms, varying in severity from mild to debilitating, with a tendency to be episodic.
“Two extreme varieties of IBS are commonly seen, with a spectrum of shades in between. The “spastic colon” type of IBS is characterized by alternating constipation and diarrhoea, associated with and often triggered by eating. The other extreme takes the form of a painless and often uncontrollable diarrhoea. This type of IBS, known as mucous colitis, is a functional disturbance in which the colon secretes abnormally large amounts of mucus that appears in the stools.”¹
IBS symptoms include:
- Irregular bowel movements, diarrhoea and/or constipation or alternating episodes of diarrhoea and constipation.
- Irregular stool formation, such as small droppings or pencil-thin and ribbon-like.
- Lower abdominal pain of a colicky nature, usually relieved by defaecation and worse after eating.
- Bloating that often worsens as the day progresses.
- Rectal mucus.
- Flatulence, occasionally reflux and/or heartburn.
- Stress, anxiety, headaches and fatigue.
A doctor may diagnose IBS when the first two or three of the above symptoms have been present for six or more months, and other more serious conditions, such as Colorectal Cancer and Crohn’s disease, have been ruled out. Conventional medicine has no cure for IBS and treatment is focused on relieving symptoms.
Possible Causes of IBS
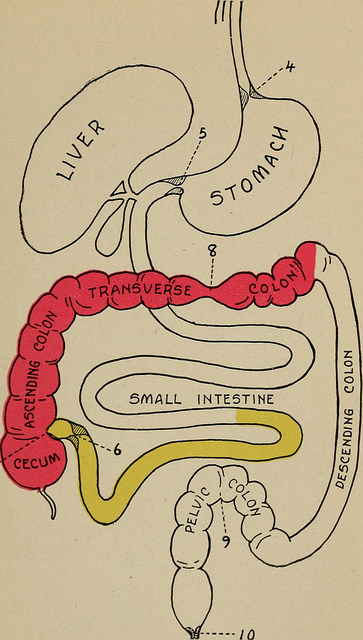
The main task of the large intestine/bowel is to convert the liquid chyme passed from the small intestine into a firm stool that can be excreted without pain or discomfort. As such, the energy of the bowel is transformative, when it is impacted with old faecal matter, toxins accumulate and imbalances can result anywhere throughout the body.
Physical symptoms are outward manifestations of inner processes; they reflect the root causes of emotional and mental imbalance within. At the heart of vitalistic and holistic medicine is the belief that the body is always striving towards health; symptoms guide our attention to areas that are in need of cleansing and strengthening. IBS is a chronic condition with acute episodes, which suggests deep-seated imbalances that can be overly responsive or sensitive to physical, emotional and mental triggers/stresses.
Physical
Problems in the gastrointestinal system most often begin with the food we eat and drink. “All maladies are due to the lack of certain food principles, such as mineral salts or vitamins, or to the absence of the normal defences of the body, such as the natural protective flora.”² A diet consisting mainly of meat and cooked and processed foods, and lacking in whole grains and fibre from fruits and vegetables, will deplete the body’s store of digestive enzymes and overload the body with toxins. The bowels require a constant supply of water on a daily basis for nutrient absorption and stool formation. Low water intake is a common cause of both constipation and diarrhoea.
You need a clean and healthy colon to assimilate nutrients and dispose of waste.³
Brian Clement
Impaired functioning anywhere in the gastrointestinal tract between the mouth and the anus will affect the lower bowel; however the pancreas, liver, and gallbladder directly influence bowel functioning through the secretion and utilisation of gastric juices and bile. Intolerance for foods such as wheat, dairy, sugar and caffeine may trigger diarrhoea. Common physical triggers for gas and bloating include bad food combinations, such as protein with starches, also overeating and eating while stressed or in a rush.
A person suffering ongoing abdominal pain and bloating is susceptible to developing a habit of poor posture, which can put pressure on internal organs. A sedentary lifestyle would indicate a need for exercise; it increases circulation, oxygenates inner organs and promotes peristalsis. Exercise also relieves stress and improves our mental outlook. When looking for the physical root causes for IBS emotional and mental stress is also a key factor, stress slows the digestive system until calm is restored. Relaxation and getting a good night’s sleep allows the body time to repair and revitalise.
Emotional
The natural energy flow of the bowel is to move forward and facilitate release. Constipation is holding back, while diarrhoea, ironically called the runs, is an effort to keep everything (liquid chyme) just as it is. An unwillingness to let go of the past can keep us from fully experiencing the present and can generate fear of an uncertain future.
Constant worry can offer the perfect distraction from taking responsibility for where we are in life right now. Habitual stress will cause regular disturbances within the gastrointestinal tract. Emotions stored in the body can contribute to physical cramping via taut contracted muscles holding onto spent emotions, past experiences, and negative behaviours. Resisting release is another holding pattern that uses up vital energy in a non-productive way.
Mental
Efforts to restrain/control life via the flow of energy within the body will inevitably lead to stagnation. Letting go and embracing change is a recurring challenge throughout all phases of life. The IBS sufferer may declare: “I’m not ready yet!” All the while stressing over what to hold on to and what to let go of. Living in the past, holding back for fear of rejection, and routinely avoiding risk will inhibit the willingness to forgive and close the mind to original ideas and new opportunities.
I don’t know why, but people of our culture have a deep-seated reluctance to relate to the colon or it’s functions.4
Isabel Moser
Taking responsibility for our thoughts is the first step towards being responsible for our actions. By cultivating a positive mental attitude, being open to new perspectives and exploring the power of our thoughts to influence emotional and physical health, we can initiate healing, clear mental stagnation, and re-connect to a sense of purpose.
Herbal Medicine for IBS
Herb classifications for IBS
- Astringents: Reverse the effects of diarrhoea and tone tissue.
- Carminatives: Relieve flatulence and associated cramping.
- Antispasmodics: Where voluntary and involuntary muscular spasms restrict circulation antispasmodics relax tension, ease abdominal cramping, griping in the bowel and restore the flow of vitality.
- Demulcents combine well with antispasmodics in easing physical distress. Their mucilaginous properties soothe and heal impaired tissue and assist with carrying waste out of the body.
- Nervines: Restore emotional and mental equilibrium, which benefits digestion.
- Bitters: To heal the liver and pancreas, promote the secretion of digestive juices
and restore normal bowel functioning. - Stimulants: To increase circulation and the uptake of other herbs in the formula.
- Anti-inflammatories: To reduce inflammation.
- Cholagogues: Most are bitter and stimulate bile flow, which promotes peristalsis.
- Aperients: Gentle laxatives for constipation dominated IBS, used in small part so as not to offset diarrhoea.
- Vulneraries: Repair damaged tissue, e.g.: if there is evidence of blood in the stool.
- Styptics to stop any bleeding.
- Antibacterial herbs to kill infection.
- Antifungal herbs to deal with fungal infections like candida.
- Vermifuges if there is evidence of parasites, e.g.: itchy anus.
- Vermicides might be reserved until it is safe to use cathartics, or alongside demulcents/mucilaginous herbs to expel waste materials from the body.
- Alteratives to cleanse the blood and reduce levels of toxaemia.
Some specific herbs …
Red Raspberry leaves are astringent, tonic and antiseptic, and also nutritive which is important when treating diarrhoea, as there is likely to be poor uptake of nutrients due to food passing through the body too quickly to be assimilated. Red Raspberry is also alterative, another desirable action where there is a build-up of toxins in the lower bowel.
Wild Yam is anti-spasmodic, anti-inflammatory, hepatic and cholagogue. “Very relaxing and soothing to the nerves. … Will expel gas from the stomach and bowels.”5
Marshmallow root contains 18-35% mucilage. “Its abundance of mucilage makes Marshmallow an excellent demulcent that is indicated wherever such an action is called for. … All inflammatory conditions of the G-I tract will benefit from its use”6
Cascara sagrada is a tonic for the peristaltic muscles. “It increases the secretions of the stomach, liver and pancreas, and is very remarkable in its action in torpor of the colon and constipation. It is, unquestionably, one of the very best and safest laxatives ever discovered.”7
Barberry as a cholagogue and hepatic increases the flow of bile, which is the body’s own natural laxative. It is also alterative, antiseptic and tonic. Carminatives are indicated alongside cholagogues to offset resultant gas and relieve associated cramping.
Fennel is the carminative of choice to relieve flatulence, indigestion, colicky cramps and bowel spasms. Lemon Balm is a carminative and anti-spasmodic, anti-depressive, anti-microbial and hepatic and works well where stress is dominant.
Ginger is a warming stimulant to increase the efficacy of companion herbs in a formula. It is known to bring everything southwards, it eases nausea and dissolves gas and is effective in relieving cramps and pains.
Gentian root is a strong bitter with an affinity for the pancreas, liver and gallbladder. It is also antiseptic, vermifuge and antispasmodic, it balances stomach acid and reduces cravings for sweet things. “Gentian is one of the most useful of our bitter vegetable tonics. It is specially useful in states of exhaustion from chronic disease and in all cases of general debility, weakness of the digestive organs and want of appetite.”8
Herbal treatment for IBS: considerations
IBS generally requires a two-stage response. The aim of the first stage is to calm inflammation, relieve discomfort and reduce stress. When diarrhoea is dominant, astringent and carminative herbs will lead, usually in a tincture along with nervines to reduce stress, bitters to stimulate digestion and stimulants to increase uptake. Antibacterial and anti-microbial herbs can be included if infection or pathogens are suspected.
When constipation is dominant, a cholagogue such as Barberry may be used to promote peristalsis or a mild aperient such as Turkey Rhubarb in a very small part, with greater parts of antispasmodic and carminative herbs. These can be administered in powder form as a bowel tonic and taken in small doses, such as ¼ teaspoon or less at a time.
Marshmallow combines well with Slippery Elm in treating mucous colitis and could be given alongside other herbs in a Nutritive Gruel to start toning and strengthening the bowels. The mucilaginous properties will absorb and eliminate mucous from the intestinal system, help to regulate intestinal flora and exert a demulcent/vulnerary action.
It is essential to start correcting dietary errors, especially emphasising the importance of drinking two to three litres of water per day. Cabbage juice and other green juices increase enzyme activity and improve digestion. Getting at least 30 minutes per day of outdoor physical exercise will also get the bowels moving. Warm infusions of relaxing herbs such as Lemon balm, Chamomile, Wood Betony and Mugwort offer an ideal way to de-stress on emotional and mental levels, while calming digestion and increasing fluid intake.
Once inflammation is reduced and diarrhoea is under control, the second stage of treatment can begin. Stage two focuses on cleansing, toning and patiently restoring normal bowel functioning. It can take 6-9 months of slowly increasing cathartics in small measures so as not to trigger a recurrence of diarrhoea, to thoroughly cleanse the bowel of accumulated faecal matter. IBS is so disruptive to the normal flow of life that most people will make the necessary commitments to lifelong dietary and lifestyle changes.
Cautions:
The presenting symptoms for Colorectal Cancer are similar to IBS, but symptoms may be of recent development and will tend to be progressive. IBS is chronic and will have a history of recurrences that may be connected to emotional/mental upsets and food sensitivities. Symptoms to look out for are: unexplained weight loss, blood in stools, family history of Colorectal cancer, Celiac disease or Inflammatory Bowel Disease (IBD), nocturnal symptoms and fever accompanying lower abdominal pain.
- Do not self-diagnose, consult an herbalist. Herbal prescriptions work best when individually formulated to respond to each client’s dominant symptoms, history and vitality.
- When diarrhoea is the dominant symptom it may be prudent to focus on dietary changes such as enzyme-rich foods and adequate hydration, daily exercise, massage, castor oil packs and other healing protocols to gradually cleanse and strengthen the bowel before administering even the mildest of laxatives.
- Due to their tannins, large doses of astringent herbs can be toxic to the liver, emphasising the need to consult a herbalist who is knowledgeable in the safe use of herbs. (Do not suppose that herbs are unsafe because of this cautionary note, remember that too much salt can also be toxic.)
- When treating IBS it is important to get the right balance of carminatives to cathartics to offset any discomfort.
- Demulcents and antispasmodics are essential to ease the discomfort of inflammation, reduce nervous cramping and griping in the lower bowel.
- It is important to increase your water intake when taking bowel herbs, and to be mindful of the risks of becoming dehydrated during bouts of diarrhoea and constipation.
- Do not take bowel herbs during pregnancy or if using an I.U.D.
- Caution is advised if you are taking contraceptive pills, or other medications, as bowel herbs may flush the pills from your system before they have time to take effect.
- Other medications/drugs should be taken separately at different times to taking herbs.
The above information is for informational purposes only and is not to be taken as medical advice.
REFERENCES:
(1) Hoffmann D. Medical Herbalism. Rochester, Vermont. Healing Arts Press; 2003. P. 276.
(2) Moser I. A., Solomon S. How and When to Be Your Own Doctor. 1997. Available at: http://soilandhealth.org/wp-content/uploads/02/0201hyglibcat/020102moser/020102Moser00toc.html P. 112. (accessed 21 June 2016)
(3) Clement B. Living Foods For Optimum Health. New York, N.Y. Three Rivers Press, 1998. P. 133.
(4) Moser I. A., Solomon S. How and When to Be Your Own Doctor. 1997. P. 118.
(5) Kloss J. Back to Eden. 2nd edition. Twin Lakes USA: Lotus Press; 2009. P. 198.
(6) Hoffmann D. Medical Herbalism. Rochester, Vermont. Healing Arts Press; 2003. P. 526.
(7) Christopher J.R. Does Your Colon Feed or Poison You? Dr. Christopher’s Newsletter, 1-1. Available at: http://www.herballegacy.com/Colon_Newsletter.html (accessed 21 June 2016)
(8) Grieve M. Gentians. A Modern Herbal. Available at: http://www.botanical.com/botanical/mgmh/g/gentia08.html (accessed 21 June 2016)
Image source: https://www.flickr.com/photos/internetarchivebookimages/14592974279/in/photostream/